Decoding Post Herpetic Neuralgia With ICD-10 Codes
Post Herpetic Neuralgia ICD-10
Post-herpetic neuralgia (PHN) is a painful condition that occurs as a complication of shingles, which is caused by the varicella-zoster virus. PHN is characterized by persistent nerve pain that lasts for months or even years after the shingles rash has healed. The condition can be debilitating and significantly impact a person’s quality of life.
Code Information

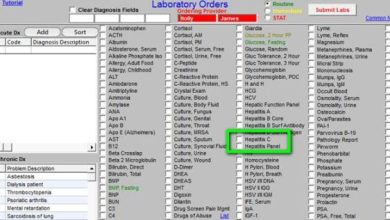
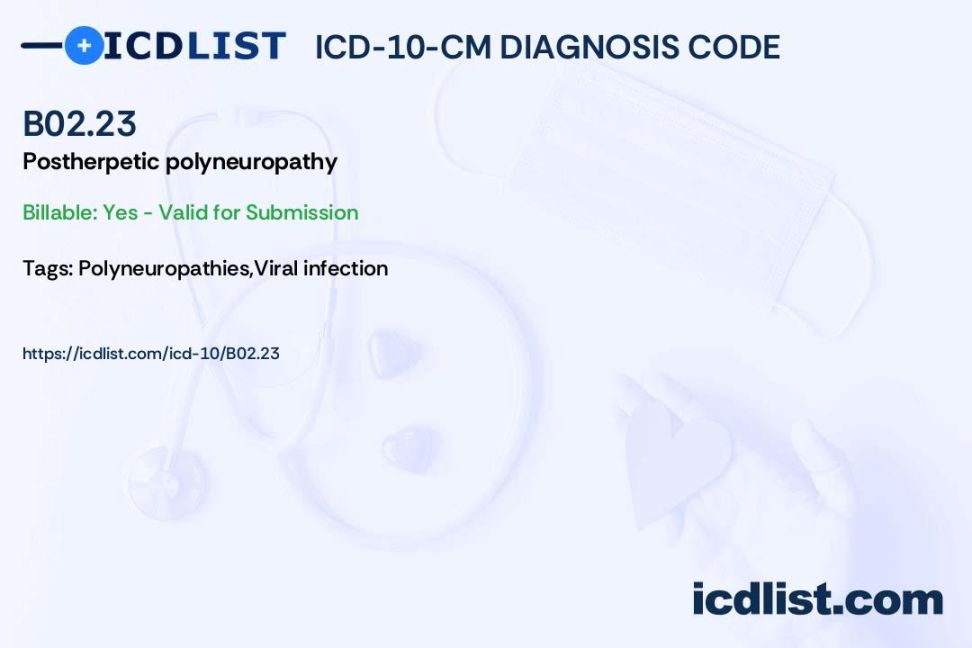
The ICD-10 code for post-herpetic neuralgia is G53.0. This code is used to classify and code for the condition in medical billing and coding systems. It is important for healthcare providers to accurately document and code for PHN to ensure proper reimbursement and tracking of the condition.
Diagnostic Related Groups (MS-DRG)
Post-herpetic neuralgia falls under the neurology DRG in the Medicare Severity Diagnosis-Related Grouping (MS-DRG) system. This grouping helps classify patients with similar diagnoses and treatments for reimbursement purposes.
Convert to ICD-9 Code
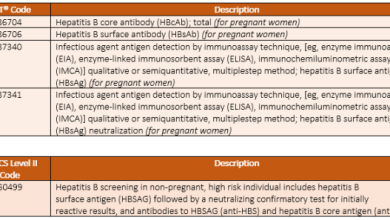
In the ICD-9 coding system, post-herpetic neuralgia is classified under code 053.19. Healthcare providers may need to convert codes from ICD-10 to ICD-9 for certain billing and coding purposes.
Code History
The ICD-10 code for post-herpetic neuralgia was implemented in October 2015 as part of the transition from ICD-9 to ICD-10 coding systems. The new code provided more specificity and accuracy in coding for PHN.
Approximate Synonyms
Other terms that may be used interchangeably with post-herpetic neuralgia include herpes zoster pain, post-shingles pain, and chronic post-herpetic neuralgia. These terms all refer to the persistent nerve pain that follows a shingles outbreak.
Clinical Information
Post-herpetic neuralgia is thought to occur due to damage to nerve fibers during a shingles outbreak. The varicella-zoster virus, which causes chickenpox, can reactivate later in life and lead to shingles and potentially PHN. The pain is typically described as burning, sharp, or shooting, and can be constant or intermittent.
Causes
The exact cause of post-herpetic neuralgia is not fully understood, but it is believed to result from nerve damage caused by the varicella-zoster virus. Older age, a weakened immune system, and severe shingles outbreaks are risk factors for developing PHN.
Symptoms
Symptoms of post-herpetic neuralgia include persistent pain in the area where shingles occurred, sensitivity to touch, itching, numbness, and tingling. The pain may be severe and can interfere with daily activities and sleep.
Diagnosis
Diagnosing post-herpetic neuralgia typically involves a thorough medical history, physical examination, and assessment of symptoms. Healthcare providers may also perform tests such as nerve conduction studies or imaging tests to rule out other causes of nerve pain.
Treatment
Treatment for post-herpetic neuralgia aims to manage pain and improve quality of life. Options may include medications such as anticonvulsants, antidepressants, topical treatments, nerve blocks, physical therapy, and alternative therapies like acupuncture. In some cases, surgery may be recommended for severe or resistant cases of PHN.
Conclusion
Post-herpetic neuralgia is a challenging condition that requires comprehensive management to alleviate pain and improve quality of life. Accurate coding and documentation are essential for proper reimbursement and tracking of the condition in healthcare settings.
FAQs
1. Can post-herpetic neuralgia be prevented?
While there is no guaranteed way to prevent PHN, getting vaccinated against shingles can reduce the risk of developing the condition.
2. How long does post-herpetic neuralgia last?
PHN can last for months or even years after the shingles rash has healed. The duration of pain varies from person to person.
3. Is post-herpetic neuralgia curable?
While there is no definitive cure for PHN, treatment options can help manage pain and improve quality of life for individuals with the condition.