Myasthenia Gravis ICD-10: Understanding The Diagnosis And Treatment Options
What is Myesthenia Gravis ICD-10?
Myesthenia gravis is a chronic autoimmune neuromuscular disease that causes weakness in the skeletal muscles, which are responsible for breathing and moving parts of the body. The ICD-10 code for myesthenia gravis is G70.0.
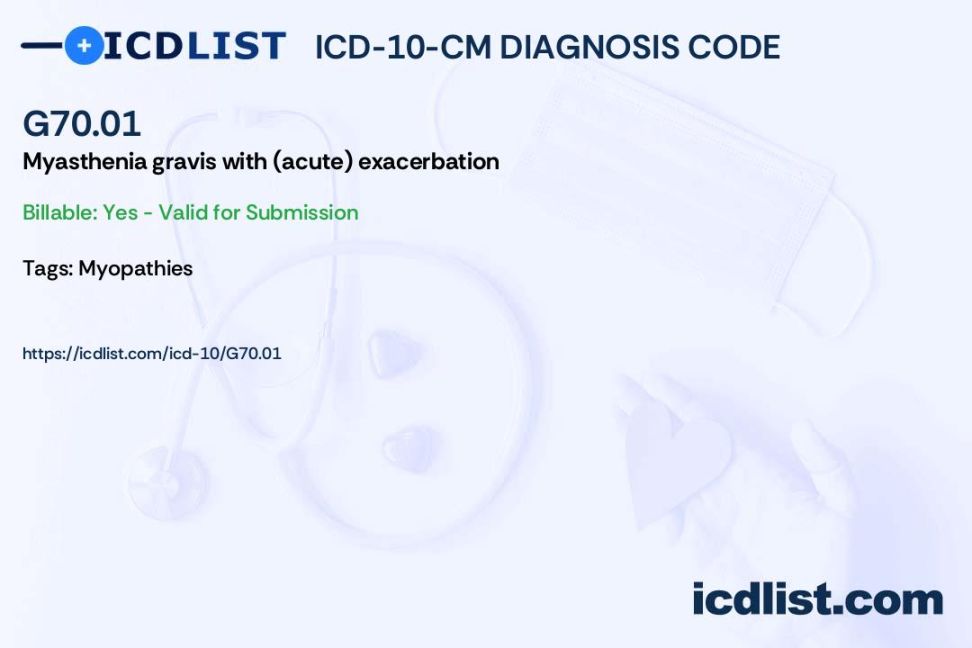
Code Information
The ICD-10 code G70.0 is used to classify myesthenia gravis, which is a rare condition that affects the communication between nerves and muscles. This code helps healthcare providers accurately diagnose and treat patients with this condition.
Diagnostic Related Groups (MS-DRG)
Myesthenia gravis is classified under MS-DRG 080, which includes diseases and disorders of the nervous system. This DRG helps hospitals and healthcare providers categorize patients with similar diagnoses for billing and administrative purposes.
Convert to ICD-9 Code
The ICD-9 code for myesthenia gravis is 358.0. This code was used prior to the implementation of ICD-10 and is still relevant for historical data and research purposes.
Code History
The ICD-10 code G70.0 for myesthenia gravis was introduced in 2016 as part of the 10th revision of the International Classification of Diseases. This code replaced the previous ICD-9 code 358.0 for this condition.
Approximate Synonyms
Myesthenia gravis may also be referred to as MG or autoimmune myesthenia. These are common synonyms used to describe the same neuromuscular disorder characterized by muscle weakness.
Clinical Information
Myesthenia gravis is caused by a breakdown in communication between nerves and muscles, leading to muscle weakness and fatigue. This condition can affect any skeletal muscle in the body, including those involved in breathing and swallowing.
Causes
The exact cause of myesthenia gravis is unknown, but it is believed to be an autoimmune disorder where the immune system mistakenly attacks the neuromuscular junction. This results in decreased signaling between nerves and muscles, leading to muscle weakness.
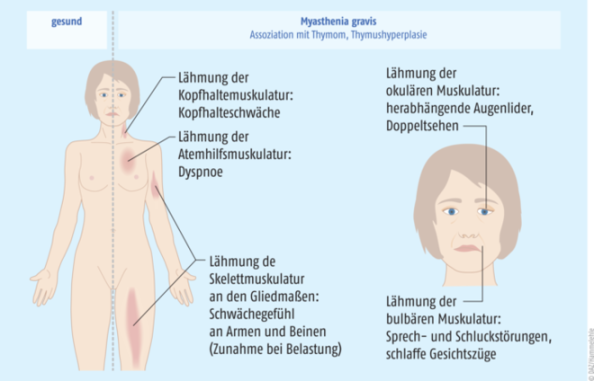
Symptoms
Common symptoms of myesthenia gravis include muscle weakness, fatigue, drooping eyelids, double vision, difficulty speaking, chewing, swallowing, and breathing. Symptoms may worsen with physical activity and improve with rest.
Diagnosis
Diagnosis of myesthenia gravis typically involves a physical exam, medical history review, blood tests to check for antibodies, nerve conduction studies, electromyography, and a Tensilon test to assess muscle strength and function.
Treatment
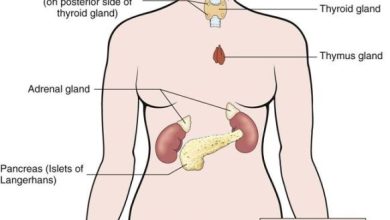
Treatment for myesthenia gravis aims to manage symptoms, improve muscle strength, and maintain quality of life. Common treatments include medications to suppress the immune system, improve nerve-muscle communication, and manage symptoms. In severe cases, surgery to remove the thymus gland may be recommended.
Conclusion
Myesthenia gravis is a chronic autoimmune neuromuscular disease that causes muscle weakness and fatigue. The ICD-10 code G70.0 is used to classify this condition, which can be managed with medications, therapy, and surgery. Early diagnosis and treatment are key to improving quality of life for individuals with myesthenia gravis.
FAQs
1. Can myesthenia gravis be cured?
Myesthenia gravis is a chronic condition that can be managed but not cured. Treatment aims to control symptoms and improve quality of life.
2. Is myesthenia gravis hereditary?
While myesthenia gravis is not directly inherited, there may be a genetic predisposition that increases the risk of developing this condition.
3. Can myesthenia gravis affect children?
Myesthenia gravis can affect individuals of any age, including children. Early diagnosis and treatment are essential for managing symptoms in pediatric patients.
4. Are there any lifestyle changes that can help manage myesthenia gravis?
Staying active, eating a healthy diet, getting enough rest, and avoiding stress can help manage symptoms of myesthenia gravis and improve overall well-being.
5. What specialists should I see for myesthenia gravis?
Individuals with myesthenia gravis may benefit from seeing a neurologist, immunologist, or rheumatologist for specialized care and treatment.