Cracking The Code: Understanding Carotid Arterial Disease ICD-10 Diagnosis
What is Carotid Arterial Disease ICD 10?
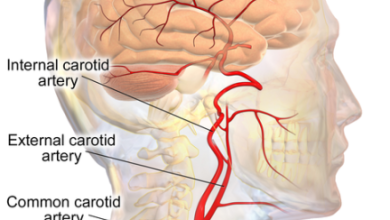
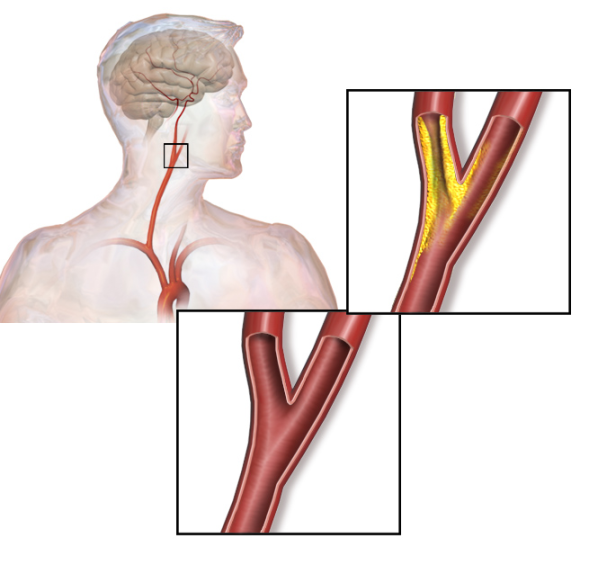
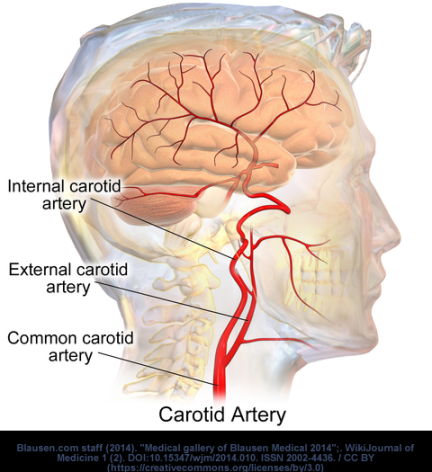
Carotid arterial disease is a condition that involves the narrowing or blockage of the carotid arteries, which are the main blood vessels that supply oxygen-rich blood to the brain. In the ICD-10 coding system, carotid arterial disease is classified under the code I63.0.
Code Information
The ICD-10 code for carotid arterial disease is used by healthcare providers to accurately diagnose and document the condition in medical records. This code helps in tracking the prevalence of the disease, monitoring treatment outcomes, and determining appropriate reimbursement for healthcare services.
Diagnostic Related Groups (MS-DRG)
The diagnosis of carotid arterial disease falls under the MS-DRG 061 category, which includes disorders of the circulatory system. This DRG grouping helps in the classification of patients for the purpose of reimbursement and resource allocation in healthcare facilities.
Convert to ICD-9 Code
In the ICD-9 coding system, carotid arterial disease is classified under the code 433.10. It is important for healthcare providers to accurately convert the diagnosis to the appropriate ICD-9 code for billing and reporting purposes.
Code History
The ICD-10 code for carotid arterial disease was introduced in 2015 as part of the transition from the ICD-9 coding system. The new code provides more specific and detailed information about the condition, improving accuracy in diagnosis and treatment.
Approximate Synonyms
Other terms used to describe carotid arterial disease include carotid artery stenosis, carotid artery occlusion, and carotid artery atherosclerosis. These synonyms are used interchangeably in medical literature and coding systems.
Clinical Information

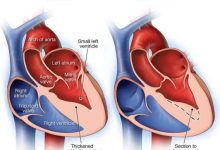
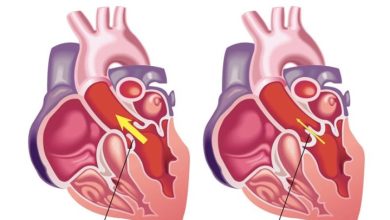
Carotid arterial disease is commonly caused by atherosclerosis, a condition where plaque builds up in the arteries, leading to narrowing and reduced blood flow. This can increase the risk of stroke, transient ischemic attacks, and other cardiovascular complications.
Causes
The primary cause of carotid arterial disease is atherosclerosis, which is associated with risk factors such as high cholesterol, high blood pressure, smoking, diabetes, and obesity. Genetics and age also play a role in the development of the condition.
Symptoms
Patients with carotid arterial disease may experience symptoms such as transient ischemic attacks (TIAs), also known as mini-strokes, sudden weakness or numbness on one side of the body, trouble speaking or understanding speech, and vision problems. Severe cases can lead to strokes.
Diagnosis
Diagnosis of carotid arterial disease is typically done through imaging tests such as carotid ultrasound, magnetic resonance angiography (MRA), computed tomography angiography (CTA), and carotid angiography. These tests help in evaluating the extent of blockage in the arteries.
Treatment
Treatment for carotid arterial disease may include lifestyle modifications such as quitting smoking, eating a healthy diet, exercising regularly, and managing underlying conditions like high blood pressure and diabetes. In severe cases, medication, surgery, or minimally invasive procedures may be recommended.
Conclusion
Carotid arterial disease is a serious condition that can lead to life-threatening complications such as stroke if left untreated. It is important for healthcare providers to accurately diagnose and document the condition using the ICD-10 code to ensure appropriate treatment and monitoring of patients.
FAQs
1. What are the risk factors for carotid arterial disease?
Risk factors for carotid arterial disease include high cholesterol, high blood pressure, smoking, diabetes, obesity, genetics, and age.
2. How is carotid arterial disease diagnosed?
Carotid arterial disease is diagnosed through imaging tests such as carotid ultrasound, magnetic resonance angiography (MRA), computed tomography angiography (CTA), and carotid angiography.
3. What are the symptoms of carotid arterial disease?
Symptoms of carotid arterial disease include transient ischemic attacks (TIAs), sudden weakness or numbness, trouble speaking, and vision problems.