Decoding Granulomatosis With Polyangiitis: Understanding ICD-10 Codes
Granulomatosis with Polyangiitis ICD-10
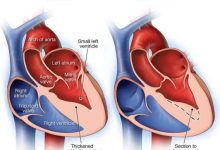
Granulomatosis with polyangiitis, also known as Wegener’s granulomatosis, is a rare autoimmune disease that causes inflammation of blood vessels in the nose, sinuses, throat, lungs, and kidneys. It is characterized by the formation of granulomas, which are small clusters of immune cells that can damage blood vessels and surrounding tissues.
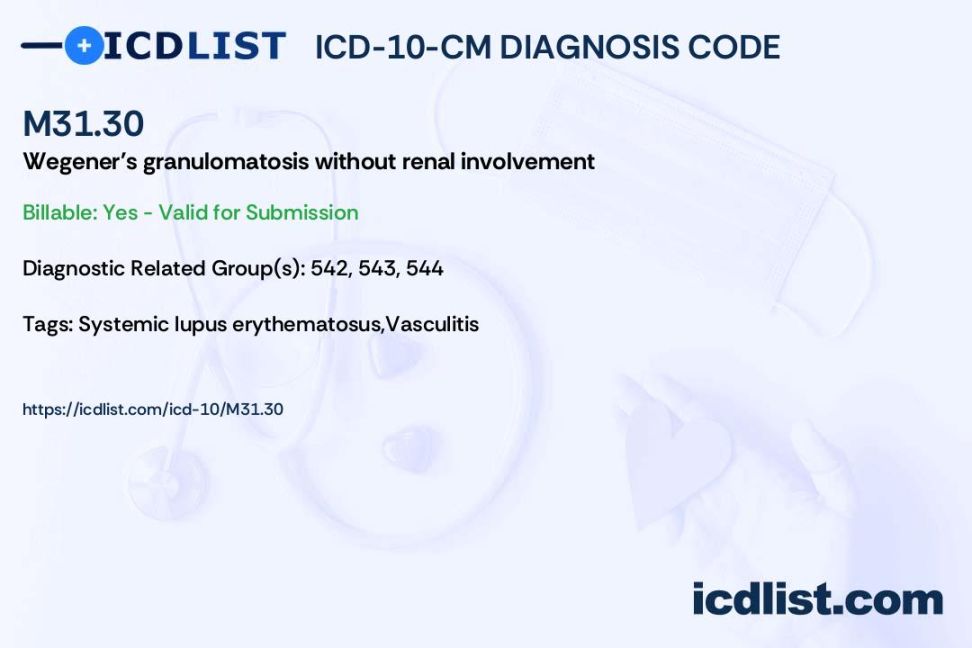
Code Information: The ICD-10 code for granulomatosis with polyangiitis is M31.31.
Diagnostic Related Groups (MS-DRG): The MS-DRG for granulomatosis with polyangiitis is 813 – Red blood cell disorders with MCC.
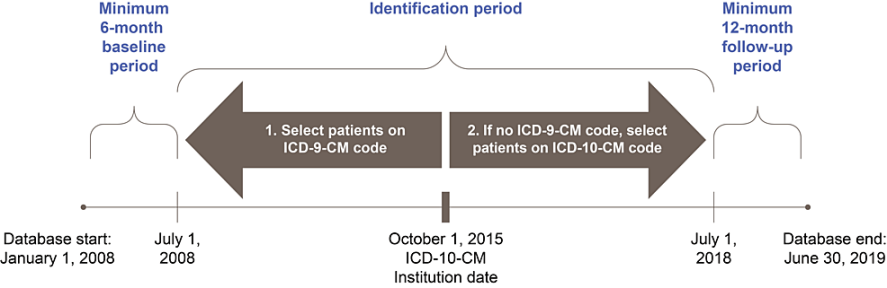
Convert to ICD-9 Code: The ICD-9 code for granulomatosis with polyangiitis is 446.4.
Code History: The ICD-10 code for granulomatosis with polyangiitis was implemented on October 1, 2015.
Approximate Synonyms: Other names for granulomatosis with polyangiitis include Wegener’s granulomatosis, GPA, and ANCA-associated vasculitis.
Clinical Information: Granulomatosis with polyangiitis is a systemic vasculitis that primarily affects small and medium-sized blood vessels. It can lead to tissue damage and organ dysfunction if left untreated.
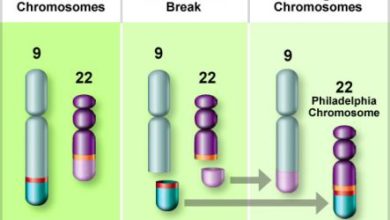
Causes: The exact cause of granulomatosis with polyangiitis is unknown, but it is believed to be triggered by a combination of genetic and environmental factors. It is also associated with the presence of anti-neutrophil cytoplasmic antibodies (ANCAs).
Symptoms: Common symptoms of granulomatosis with polyangiitis include sinus pain and congestion, nosebleeds, coughing up blood, chest pain, shortness of breath, joint pain, and kidney problems.
Diagnosis: Diagnosis of granulomatosis with polyangiitis typically involves a physical examination, blood tests to detect ANCA antibodies, imaging studies such as X-rays or CT scans, and a biopsy of affected tissue.
Treatment: Treatment for granulomatosis with polyangiitis often involves a combination of corticosteroids, immunosuppressant drugs, and biologic therapies to reduce inflammation and prevent further damage to organs. In severe cases, surgery may be necessary to repair damaged blood vessels or organs.
In conclusion, granulomatosis with polyangiitis is a rare but serious autoimmune disease that can affect multiple organs and lead to significant morbidity if not properly managed. Early diagnosis and treatment are essential to improving outcomes and preventing long-term complications.
FAQs:
1. Can granulomatosis with polyangiitis be cured? Unfortunately, there is no cure for granulomatosis with polyangiitis, but treatment can help manage symptoms and prevent complications.
2. Is granulomatosis with polyangiitis a hereditary condition? While the exact cause of granulomatosis with polyangiitis is unknown, there is no evidence to suggest that it is directly inherited.
3. How is granulomatosis with polyangiitis different from other types of vasculitis? Granulomatosis with polyangiitis is characterized by the presence of granulomas and is typically associated with ANCA antibodies, which distinguish it from other forms of vasculitis.
4. Can granulomatosis with polyangiitis affect children? While granulomatosis with polyangiitis is more common in adults, it can also affect children, although it is rare in this age group.
5. What is the prognosis for patients with granulomatosis with polyangiitis? The prognosis for patients with granulomatosis with polyangiitis varies depending on the severity of the disease and how well it responds to treatment. With proper management, many patients can achieve remission and lead relatively normal lives.