Hashimoto’s Thyroiditis Icd 10
Unpacking ICD-10: E06.3 – Unveiling the Mystery of Hashimoto’s Thyroiditis
Imagine a vast library filled with countless books, each containing a unique story. In the realm of medicine, the International Classification of Diseases, 10th Revision (ICD-10) serves a similar purpose. This extensive reference system acts as a language, assigning specific codes to various medical conditions. Today, we embark on a journey to decipher code E06.3, a key that unlocks the door to understanding Hashimoto’s Thyroiditis, an intriguing autoimmune condition.
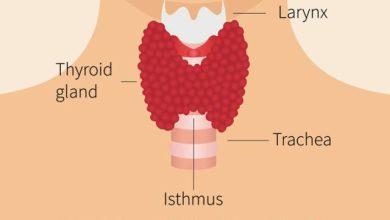
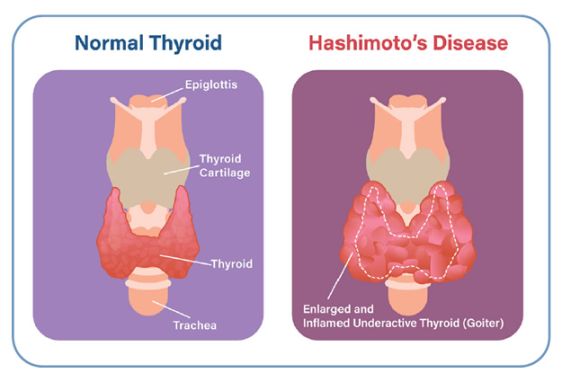
Hashimoto’s Thyroiditis, often simply called Hashimoto’s, presents a captivating narrative of the intricate interplay between the body’s immune system and the butterfly-shaped thyroid gland nestled in our throat. The thyroid gland, a diligent worker, tirelessly produces hormones that act as the body’s maestros, regulating metabolism and influencing everything from our energy levels to our body temperature. But in the curious case of Hashimoto’s, the plot thickens. The immune system, tasked with protecting us from invaders, mistakenly identifies the thyroid as a sneaky villain, launching an all-out attack. This misplaced aggression disrupts the thyroid’s hormone production, leading to a domino effect of symptoms that can leave us feeling sluggish, achy, and under the weather.
Deciphering the code E06.3 allows healthcare professionals to accurately diagnose Hashimoto’s and chart a course towards effective treatment. Imagine a detective meticulously examining a fingerprint at a crime scene. The unique pattern of the fingerprint provides crucial clues, just like the specific code in ICD-10. With this knowledge in hand, doctors can employ various tools like blood tests and imaging techniques to gather more evidence and confirm the presence of Hashimoto’s.
Unmasking the Culprit: Unveiling the Roots of Hashimoto’s
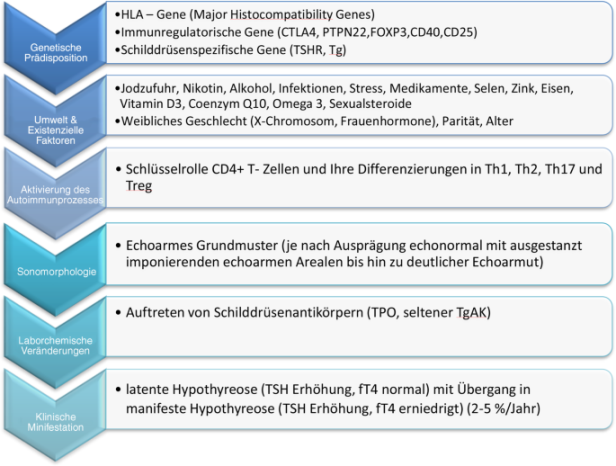
While the exact cause of Hashimoto’s remains an elusive puzzle, scientists have pieced together some intriguing clues. Genetics appear to play a role, with certain genes increasing the susceptibility to the condition. Environmental factors may also be involved, with exposure to toxins or viruses potentially triggering the immune system’s mistaken identity crisis.
The Body Fights Back: Exploring the Immune System’s Misguided Mission
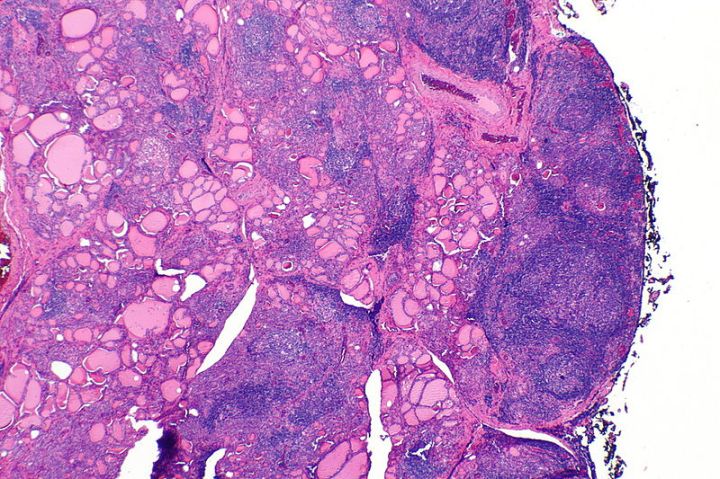
The immune system, our body’s valiant defender, is usually adept at distinguishing friend from foe. However, in Hashimoto’s, this loyal protector turns into an overzealous guard dog. Cells within the immune system, called lymphocytes, mistake the healthy thyroid tissue for a foreign invader. These rogue lymphocytes launch an attack, producing antibodies that damage the thyroid gland and hinder its hormone production.
A Symphony of Hormones: Understanding the Impact on Our Wellbeing
The thyroid gland, resembling a tiny butterfly, conducts a symphony of hormones essential for our well-being. The maestro of this orchestra is thyroxine, often abbreviated as T4. T4 plays a critical role in regulating metabolism, influencing how our bodies convert food into energy. Another crucial hormone, triiodothyronine (T3), acts like a potent violinist, fine-tuning the body’s metabolic processes.
In the chaos of Hashimoto’s, the disruption of hormone production creates a discord within the body’s symphony. The insufficient production of T4 and T3 disrupts the delicate balance of metabolism, leading to a cascade of symptoms. Individuals with Hashimoto’s may experience fatigue, muscle weakness, unexplained weight gain, and difficulty concentrating, all stemming from the imbalance created by the malfunctioning thyroid gland.
Restoring the Harmony: Exploring Treatment Options
Fortunately, with the help of medical professionals, individuals with Hashimoto’s can reclaim their health and well-being. Treatment typically involves synthetic thyroid hormone replacement therapy. By introducing the missing hormones back into the body, doctors can restore the balance and alleviate the symptoms of Hashimoto’s. This allows the body to return to a state of homeostasis, where all the parts work together in harmony.
Living Well with Hashimoto’s: Embracing a Balanced Lifestyle
While there is no cure for Hashimoto’s, maintaining a healthy lifestyle can play a vital role in managing the condition. A balanced diet rich in fruits, vegetables, and whole grains provides the body with the essential nutrients it needs to function optimally. Regular exercise also plays a crucial role, promoting overall well-being and improving energy levels.
A Beacon of Hope: Ongoing Research for a Brighter Future
Imagine a grand masquerade ball. Guests adorned in elegant attire, laughter echoing through the halls, a vibrant scene of revelry. But amidst the merriment, a peculiar character stands out. Dressed impeccably, they move with a certain sluggishness, their smile slightly strained. This, my friends, is Euthyroid Sick Syndrome (ESS), a guest with a hidden condition in the grand ball of Hashimoto’s Thyroiditis.
Hashimoto’s, like a mischievous host, throws a wrench into the usual hormonal rhythm. Normally, the thyroid gland, a butterfly-shaped resident of our neck, diligently produces thyroid hormones, the body’s energetic conductors. But in Hashimoto’s, the immune system, mistaking the thyroid for an unwelcome visitor, throws a tantrum, hindering its hormone production.
This hormonal disarray can manifest in a multitude of ways, much like the diverse costumes at the ball. Some guests experience the classic symptoms of an underactive thyroid – fatigue, weight gain, feeling constantly cold. But for others, the masquerade takes a more subtle turn. Enter ESS, our guest in disguise.
ESS presents a curious situation. Blood tests, the party invitations in this analogy, might show normal thyroid hormone levels, making it seem like everything’s under control. Yet, the individual struggles with symptoms that cast a shadow on their quality of life. Brain fog, like a poorly fitted mask, makes concentration difficult. Muscle aches and stiffness become unwelcome dance partners. Depression, a party crasher, might even linger at the edges of the merriment.
Here’s the twist: despite the seemingly normal hormone levels, ESS suggests a deeper dysfunction within the body’s hormonal orchestra. Imagine the music at the ball sounds off-key, despite the instruments playing the correct notes. In ESS, certain antibodies, the immune system’s overzealous security guards, might still be causing subtle disruptions, hindering the thyroid’s true potential.
Diagnosing ESS can be a challenge, requiring a keen eye for the subtlest clues. Doctors, acting as detectives at the masquerade, delve deeper than just the hormone levels. They consider the individual’s medical history, the whispers exchanged amongst different bodily systems, and the overall presentation of symptoms, like the costume and demeanor of a guest.
Fortunately, even with the mask on, ESS doesn’t have to be a permanent party spoiler. Tailored treatment plans, adjustments to medication, and a focus on healthy lifestyle choices can empower individuals to reclaim their rightful enjoyment of the ball.