Diving Into Dermatomyositis: Understanding The ICD-10 Coding Guidelines
What is Dermatomyositis?
Dermatomyositis is a rare autoimmune disease that affects the skin and muscles. It is characterized by muscle weakness and a distinctive skin rash. The exact cause of dermatomyositis is unknown, but it is believed to be related to an abnormal immune response. This condition can affect people of all ages, but it is most common in adults between the ages of 40 and 60.
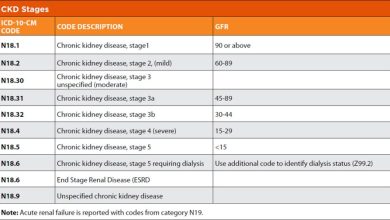
Code Information

The ICD-10 code for dermatomyositis is M33.0. This code is used to classify and code diagnoses related to dermatomyositis in medical billing and coding.
Diagnostic Related Groups (MS-DRG)

The MS-DRG for dermatomyositis is 545. This is the Medicare Severity Diagnosis-Related Group that is used to classify and reimburse hospital inpatient services for patients with dermatomyositis.
Convert to ICD-9 Code
To convert the ICD-10 code M33.0 for dermatomyositis to an ICD-9 code, you would use code 710.3. This code is used to classify and code diagnoses related to dermatomyositis in medical billing and coding under the ICD-9 system.
Code History
The ICD-10 code for dermatomyositis was first introduced in 2015 as part of the tenth revision of the International Classification of Diseases. This code replaced the previous ICD-9 code 710.3 for dermatomyositis.
Approximate Synonyms
Some approximate synonyms for dermatomyositis include inflammatory myopathy, cutaneous dermatomyositis, and idiopathic inflammatory myositis.
Clinical Information
Dermatomyositis is characterized by muscle weakness and a distinctive skin rash. The muscle weakness can affect the muscles closest to the trunk of the body, such as those in the hips, thighs, shoulders, and upper arms. The skin rash often appears on the face, neck, chest, back, and joints.
Causes
The exact cause of dermatomyositis is unknown, but it is believed to be related to an abnormal immune response. It is thought that the immune system mistakenly attacks healthy muscle and skin tissue, leading to inflammation and damage in these areas.
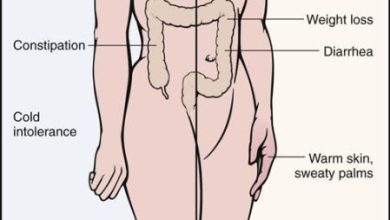
Symptoms
Common symptoms of dermatomyositis include muscle weakness, difficulty swallowing, skin rash, fatigue, weight loss, joint pain, and shortness of breath. The skin rash is often a reddish-purple color and may be itchy or painful.
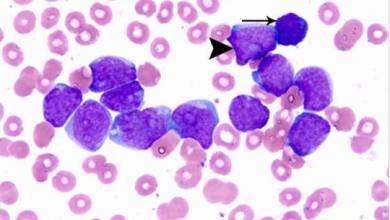
Diagnosis
Diagnosing dermatomyositis typically involves a physical examination, blood tests, and imaging studies. A muscle biopsy may also be performed to confirm the diagnosis. The characteristic skin rash and muscle weakness are key indicators of dermatomyositis.
Treatment
Treatment for dermatomyositis usually involves a combination of medications, physical therapy, and lifestyle changes. Corticosteroids are commonly prescribed to reduce inflammation and suppress the immune system. Other medications, such as immunosuppressants and antimalarial drugs, may also be used to manage symptoms.
Conclusion
In conclusion, dermatomyositis is a rare autoimmune disease that affects the skin and muscles. It is characterized by muscle weakness and a distinctive skin rash. The exact cause of dermatomyositis is unknown, but it is believed to be related to an abnormal immune response. Diagnosing and treating dermatomyositis early can help manage symptoms and improve quality of life for patients.
FAQs
1. Is dermatomyositis a hereditary condition?
No, dermatomyositis is not typically inherited and is considered to be an autoimmune disease.
2. Can dermatomyositis be cured?
There is no cure for dermatomyositis, but treatment can help manage symptoms and improve quality of life.
3. How long does it take to diagnose dermatomyositis?
Diagnosing dermatomyositis can take time, as it often requires a combination of physical exams, blood tests, and imaging studies.
4. Are there any lifestyle changes that can help manage dermatomyositis?
Maintaining a healthy diet, getting regular exercise, and avoiding stress can help manage symptoms of dermatomyositis.