Cracking The Code: Understanding Overactive Bladder ICD-10 Diagnosis
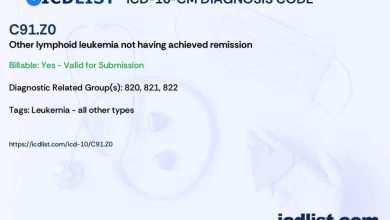
What is Overactive Bladder ICD-10 Code?
Overactive bladder (OAB) is a condition characterized by a sudden and frequent urge to urinate. It can lead to involuntary urine leakage, also known as urinary incontinence. In the International Classification of Diseases, Tenth Revision (ICD-10), the code for overactive bladder is N32.81.
Code Information
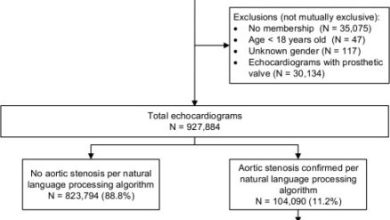
The ICD-10 code N32.81 is used to classify cases of overactive bladder in medical records. This code helps healthcare providers and researchers track the prevalence and treatment of OAB, as well as monitor outcomes and trends over time.
Diagnostic Related Groups (MS-DRG)
Overactive bladder may be classified under certain Diagnosis Related Groups (DRGs) for billing and reimbursement purposes. The most relevant DRGs for OAB include DRG 698 – Other Kidney and Urinary Tract Diagnoses with MCC and DRG 699 – Other Kidney and Urinary Tract Diagnoses without MCC.
Convert to ICD-9 Code
In the Ninth Revision of the ICD (ICD-9), overactive bladder is classified under code 596.51 – Overactive bladder. It is important for healthcare providers to be able to convert between ICD-10 and ICD-9 codes for accurate coding and billing purposes.
Code History

The ICD-10 code N32.81 for overactive bladder was introduced in 2016 as part of the updated coding system. It replaced the previous ICD-9 code 596.51 and provided a more detailed and specific classification for OAB.
Approximate Synonyms
Some approximate synonyms for overactive bladder include urge incontinence, detrusor overactivity, and bladder spasms. These terms may be used interchangeably with OAB in medical literature and coding.
Clinical Information
Overactive bladder is a common condition that can significantly impact quality of life. It is characterized by symptoms such as urinary urgency, frequency, and nocturia (waking up at night to urinate). OAB can be caused by a variety of factors, including nerve damage, bladder inflammation, and muscle dysfunction.
Causes
The exact cause of overactive bladder is not always clear, but several factors may contribute to the development of this condition. These include age-related changes in bladder function, neurological disorders, urinary tract infections, and certain medications.
Symptoms
Individuals with overactive bladder may experience a range of symptoms, including a sudden and strong urge to urinate, frequent urination (more than eight times a day), and urge incontinence (leaking urine before reaching the restroom). Other symptoms may include nocturia, or waking up at night to urinate, and difficulty emptying the bladder completely.
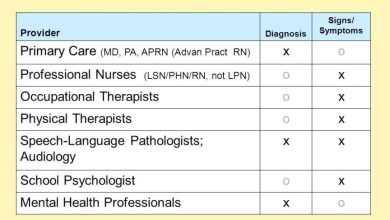
Diagnosis
Diagnosing overactive bladder typically involves a thorough medical history, physical examination, and possibly additional tests such as a urinalysis, bladder diary, or urodynamic testing. Healthcare providers may also use questionnaires to assess OAB symptoms and severity.
Treatment
Treatment for overactive bladder may include lifestyle modifications, such as bladder training, pelvic floor exercises, and dietary changes. Medications, such as anticholinergics or beta-3 agonists, may also be prescribed to help control OAB symptoms. In some cases, advanced treatments such as botulinum toxin injections or sacral neuromodulation may be recommended.
Conclusion
Overactive bladder is a common and bothersome condition that can significantly impact quality of life. Proper diagnosis and treatment are essential for managing OAB symptoms and improving overall well-being. By understanding the ICD-10 code for overactive bladder and its clinical implications, healthcare providers can better track and address this condition in clinical practice.
FAQs
Q: Is overactive bladder a common condition?
A: Yes, overactive bladder is a common condition that affects millions of individuals worldwide.
Q: What are the risk factors for developing overactive bladder?
A: Risk factors for OAB include age, gender, obesity, and certain medical conditions.
Q: Can overactive bladder be cured?
A: While there is no cure for OAB, symptoms can be effectively managed with proper treatment and lifestyle modifications.