Cracking The Code: Understanding Hashimoto’s Thyroiditis ICD-10 Classification
What is Hashimoto’s Thyroiditis ICD 10?
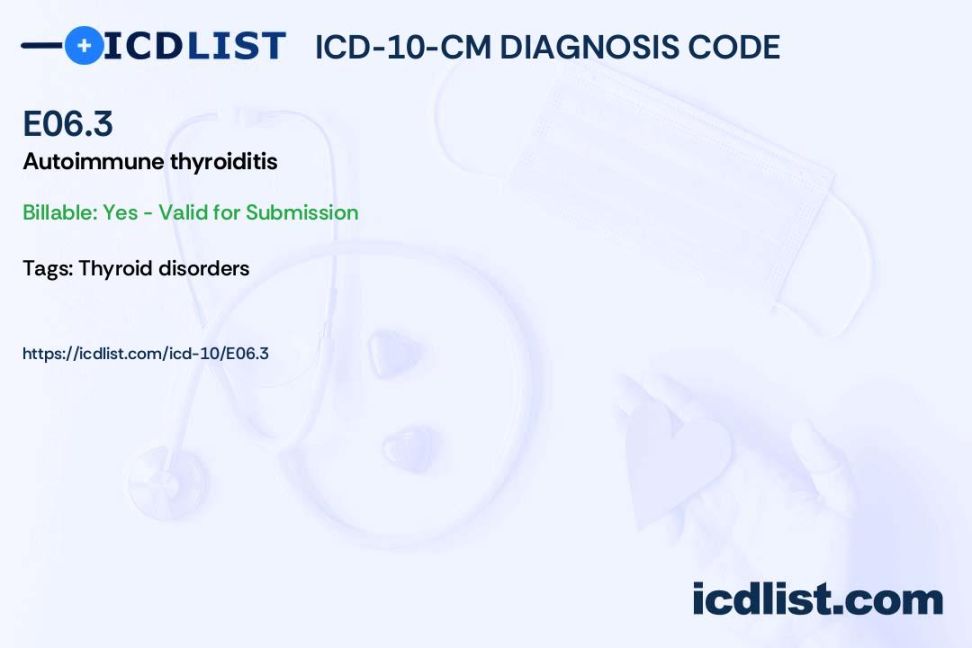
Hashimoto’s thyroiditis is an autoimmune disorder that causes inflammation of the thyroid gland, leading to an underactive thyroid or hypothyroidism. In the International Classification of Diseases, 10th Revision (ICD-10), Hashimoto’s thyroiditis is assigned the code E06.3.
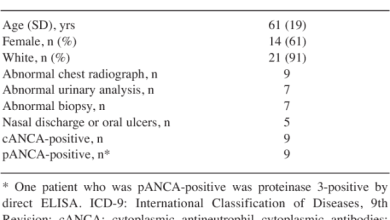
Code Information

The ICD-10 code for Hashimoto’s thyroiditis is used by healthcare providers to classify and code diagnoses in medical records for billing and statistical purposes. It helps in tracking the prevalence and incidence of the disease, as well as monitoring trends in healthcare utilization and outcomes.
Diagnostic Related Groups (MS-DRG)
Hashimoto’s thyroiditis falls under the endocrine, nutritional, and metabolic diseases MS-DRG category in the Medicare Severity-Diagnosis Related Group (MS-DRG) system. This grouping is used for inpatient hospital stays to determine payment rates based on the patient’s diagnosis and treatment.
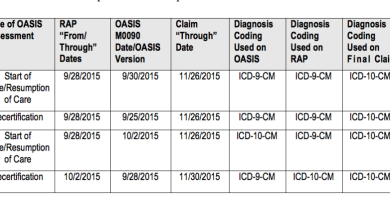
Convert to ICD-9 Code

For those familiar with the previous ICD-9 coding system, the equivalent code for Hashimoto’s thyroiditis in ICD-9 is 245.2. It is important to note that ICD-9 codes are no longer used for healthcare reporting and billing purposes, as they have been replaced by the more detailed and specific ICD-10 coding system.
Code History
The ICD-10 code for Hashimoto’s thyroiditis was introduced in 1994 and has undergone several revisions and updates since then to reflect changes in diagnostic criteria and medical knowledge. The current code, E06.3, specifically identifies Hashimoto’s thyroiditis as an autoimmune disorder affecting the thyroid gland.
Approximate Synonyms
Some approximate synonyms for Hashimoto’s thyroiditis include chronic lymphocytic thyroiditis, autoimmune thyroiditis, lymphadenoid goiter, and struma lymphomatosa. These terms may be used interchangeably to describe the same condition in medical literature and coding.
Clinical Information
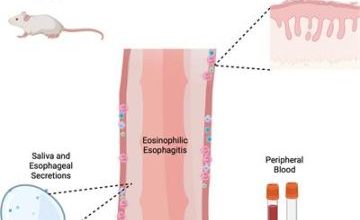
Hashimoto’s thyroiditis is characterized by the immune system attacking the thyroid gland, leading to inflammation, damage, and dysfunction of the gland. This results in a decrease in thyroid hormone production, causing symptoms of hypothyroidism such as fatigue, weight gain, cold intolerance, and depression.
Causes
The exact cause of Hashimoto’s thyroiditis is not fully understood, but it is believed to be a combination of genetic predisposition and environmental triggers. Factors such as family history of autoimmune diseases, viral infections, and hormonal imbalances may contribute to the development of the condition.
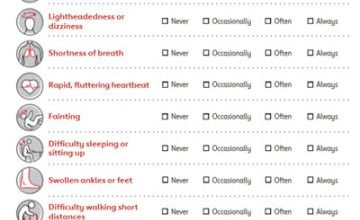
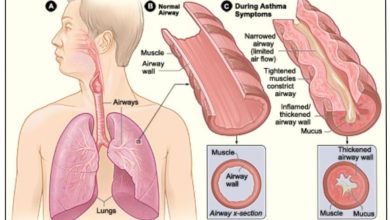
Symptoms
Common symptoms of Hashimoto’s thyroiditis include fatigue, weight gain, dry skin, hair loss, constipation, depression, and menstrual irregularities in women. Some individuals may also experience swelling of the thyroid gland or a goiter, as well as symptoms of hypothyroidism such as cold intolerance and muscle weakness.
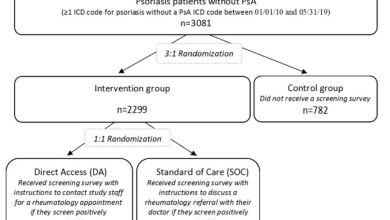
Diagnosis
Diagnosis of Hashimoto’s thyroiditis is made based on a combination of symptoms, physical examination findings, blood tests measuring thyroid function and autoantibodies, and imaging studies such as ultrasound of the thyroid gland. A healthcare provider will also consider the patient’s medical history and family history of autoimmune diseases.
Treatment
Treatment for Hashimoto’s thyroiditis typically involves lifelong thyroid hormone replacement therapy to restore normal thyroid function and alleviate symptoms of hypothyroidism. Regular monitoring of thyroid hormone levels and adjustments in medication dosage may be necessary to maintain optimal thyroid function and prevent complications.
Conclusion
Hashimoto’s thyroiditis is a common autoimmune disorder affecting the thyroid gland, leading to hypothyroidism and a range of symptoms. Proper diagnosis and management of the condition with thyroid hormone replacement therapy can help improve quality of life and prevent complications associated with untreated hypothyroidism.
FAQs
1. Is Hashimoto’s thyroiditis a hereditary condition?
2. Can Hashimoto’s thyroiditis be cured?
3. What are the risk factors for developing Hashimoto’s thyroiditis?
4. How is Hashimoto’s thyroiditis different from other thyroid disorders?
5. Are there any natural remedies or alternative treatments for Hashimoto’s thyroiditis?