Unlocking The Code: Understanding ICD-10 For Esophageal Cancer
What is Esophageal Cancer?
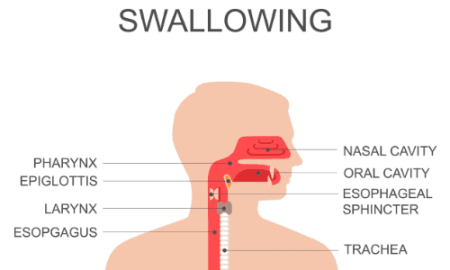
Esophageal cancer is a type of cancer that begins in the cells of the esophagus, which is the tube that carries food from the mouth to the stomach. This type of cancer can occur anywhere along the esophagus and can spread to other parts of the body if not treated early.
Code Information
The ICD-10 code for esophageal cancer is C15.9. This code is used to classify and code diagnoses and procedures for billing and statistical purposes.
Diagnostic Related Groups (MS-DRG)
Esophageal cancer is typically classified under MS-DRG 326, which includes esophagitis, gastroenteritis, and miscellaneous digestive disorders.
Convert to ICD-9 Code
If you need to convert the ICD-10 code for esophageal cancer to an ICD-9 code, the corresponding code is 150.9.
Code History
The ICD-10 code for esophageal cancer was first introduced in 2015 as part of the transition from ICD-9 to ICD-10 coding systems.
Approximate Synonyms
Some approximate synonyms for esophageal cancer include malignant neoplasm of the esophagus and esophageal carcinoma.
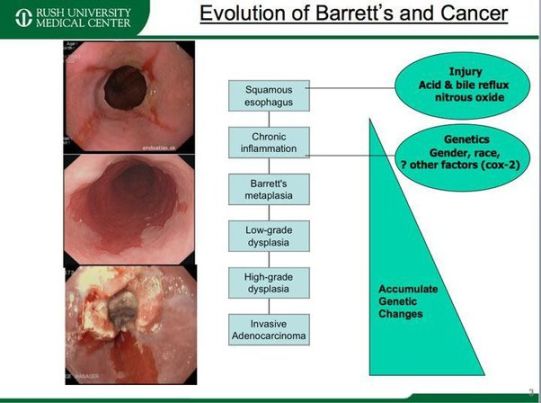
Clinical Information
Esophageal cancer is often associated with a variety of risk factors, including smoking, heavy alcohol consumption, obesity, and gastroesophageal reflux disease (GERD). The most common type of esophageal cancer is squamous cell carcinoma, followed by adenocarcinoma.
Causes
The exact cause of esophageal cancer is unknown, but it is believed to be related to a combination of genetic and environmental factors. Risk factors for developing esophageal cancer include smoking, heavy alcohol consumption, obesity, and a history of GERD.
Symptoms
Symptoms of esophageal cancer may include difficulty swallowing, chest pain, weight loss, and persistent coughing. These symptoms can vary depending on the location and stage of the cancer.
Diagnosis
Esophageal cancer is typically diagnosed through a combination of imaging tests, such as a barium swallow or CT scan, and a biopsy of the affected area. Once diagnosed, further tests may be conducted to determine the stage of the cancer and the best course of treatment.
Treatment
Treatment for esophageal cancer may include surgery, chemotherapy, radiation therapy, or a combination of these treatments. The specific treatment plan will depend on the stage of the cancer, the location of the tumor, and the overall health of the patient.
Conclusion
Esophageal cancer is a serious condition that requires prompt diagnosis and treatment. By understanding the causes, symptoms, and treatment options for esophageal cancer, patients can work with their healthcare providers to develop a comprehensive care plan that addresses their individual needs.
FAQs
Can esophageal cancer be prevented?
While there is no sure way to prevent esophageal cancer, reducing risk factors such as smoking, alcohol consumption, and obesity may help lower the risk of developing the disease.
What are the survival rates for esophageal cancer?
Survival rates for esophageal cancer vary depending on the stage of the cancer at diagnosis, but early detection and treatment can improve outcomes.
Is esophageal cancer hereditary?
While esophageal cancer can sometimes run in families, the majority of cases are not believed to be hereditary.
What are the side effects of treatment for esophageal cancer?
Common side effects of treatment for esophageal cancer may include nausea, fatigue, and hair loss, among others.
How often should I undergo screening for esophageal cancer?
It is important to discuss screening recommendations with your healthcare provider, as the frequency of screening may vary based on individual risk factors and medical history.