Navigating Primary Biliary Cholangitis ICD-10 Codes: Understanding The Diagnosis
What is Primary Biliary Cholangitis ICD-10?
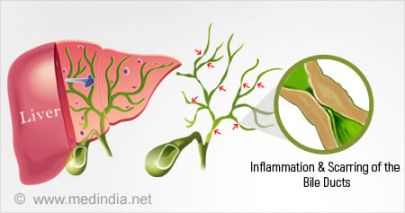
Primary biliary cholangitis, previously known as primary biliary cirrhosis, is a chronic liver disease characterized by the destruction of small bile ducts within the liver. This condition leads to a buildup of bile in the liver, causing inflammation and scarring of the liver tissue. Primary biliary cholangitis is classified under the ICD-10 code K74.3.
Code Information
The ICD-10 code for primary biliary cholangitis is K74.3. This code is used to classify and track cases of primary biliary cholangitis in medical records and billing systems. It is important to use the correct ICD-10 code when diagnosing and treating patients with primary biliary cholangitis to ensure accurate documentation and reimbursement.
Diagnostic Related Groups (MS-DRG)
Primary biliary cholangitis falls under the Medicare Severity-Diagnosis Related Group (MS-DRG) 441 – Disorders of Liver except Malignancy, Cirrhosis, Alcoholic Hepatitis. This DRG is used to categorize patients with liver disorders for billing and reimbursement purposes. Patients with primary biliary cholangitis may be assigned to this DRG based on their diagnosis and treatment.
Convert to ICD-9 Code
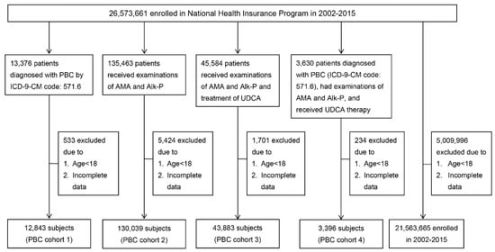
Primary biliary cholangitis was previously classified under the ICD-9 code 571.6. However, with the implementation of ICD-10 coding system, the code for primary biliary cholangitis has been updated to K74.3. It is important to use the current ICD-10 code for accurate coding and billing.
Code History
The ICD-10 code for primary biliary cholangitis, K74.3, was introduced in 2016 as part of the transition from ICD-9 to ICD-10 coding system. This change was made to improve accuracy and specificity in coding liver diseases, including primary biliary cholangitis. Healthcare providers and coders should be familiar with the updated code for proper documentation and billing.
Approximate Synonyms
Primary biliary cholangitis is also known by other names such as primary biliary cirrhosis or autoimmune cholangitis. These terms may be used interchangeably to describe the same condition characterized by the destruction of bile ducts within the liver. However, the official ICD-10 code for this condition is K74.3 – primary biliary cholangitis.
Clinical Information
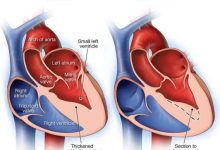
Primary biliary cholangitis is an autoimmune disease that primarily affects the liver. It is characterized by the progressive destruction of small bile ducts within the liver, leading to impaired bile flow and accumulation of toxic substances in the liver tissue. This condition can result in inflammation, scarring, and ultimately, liver failure if left untreated.
Causes
The exact cause of primary biliary cholangitis is unknown, but it is believed to be triggered by a combination of genetic, environmental, and immune factors. The immune system mistakenly attacks the bile ducts in the liver, leading to inflammation and damage. Risk factors for developing primary biliary cholangitis include being female, over the age of 40, and having a family history of autoimmune diseases.
Symptoms
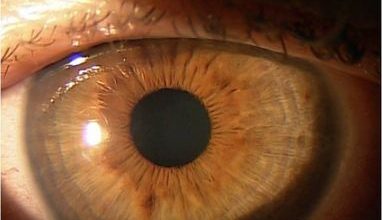
Primary biliary cholangitis is often asymptomatic in the early stages, but as the disease progresses, patients may experience symptoms such as fatigue, itching, abdominal pain, dry eyes and mouth, and yellowing of the skin and eyes (jaundice). Other symptoms may include joint pain, osteoporosis, and complications related to liver dysfunction.
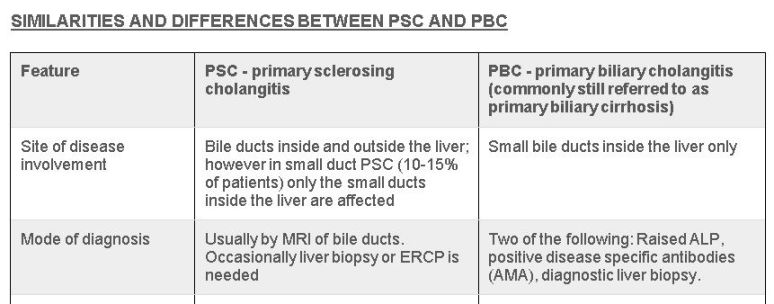
Diagnosis
Diagnosing primary biliary cholangitis typically involves a combination of medical history, physical examination, blood tests, imaging studies (such as ultrasound or MRI), and liver biopsy. Blood tests may reveal elevated liver enzymes and antibodies specific to primary biliary cholangitis. A liver biopsy can confirm the presence of bile duct damage and inflammation.
Treatment
Treatment for primary biliary cholangitis aims to slow the progression of the disease, manage symptoms, and prevent complications. This may include medications to reduce inflammation and bile buildup, relieve itching, and improve liver function. In some cases, liver transplant may be necessary for patients with advanced liver disease. Lifestyle modifications such as a healthy diet, regular exercise, and avoiding alcohol can also help manage the condition.
Conclusion
Primary